This document has been archived for historical reference. For the latest information on Metabolic and Bariatric Surgical procedures, visit our Bariatric Surgery Procedures Page in our Patient Learning Center
Chapter 1 – Introduction
Weight loss (bariatric) surgery is a unique field, in that with one operation, a person can be potentially cured of numerous medical diseases including diabetes, hypertension, high cholesterol, sleep apnea, chronic headaches, venous stasis disease, urinary incontinence, liver disease, and arthritis. Bariatric surgery is the only proven method that results in durable weight loss. This proven surgical approach, combined with the dismal failure of dieting, the marked improvement in quality of life and the quick recovery with minimally invasive techniques, has fueled the surge in the number of bariatric procedures performed annually over the last 10 years.
Weight loss operations can be divided into restrictive procedures and malabsorptive procedures. Malabsorptive procedures reduce the absorption of calories, proteins and other nutrients. In contrast, restrictive operations decrease food intake and promote a feeling of fullness (satiety) after meals. Some operations are a combination of both. The gastric bypass (open and laparoscopic), the laparoscopic adjustable band and the biliopancreatic diversion (with or without the duodenal switch) are the primary procedures used currently.
While the majority of patients who undergo these procedures are very successful, no procedure is perfect. Only through an honest discussion with a bariatric surgeon can patients decide which procedure may be best suited for them. With the development of new techniques and innovative procedures, patients and surgeons must remember the lessons learned from pioneering surgeons.
Chapter 2 – Jejunoileal Bypass
The first operations designed solely for the purpose of weight loss were initially performed in the 1950s at the University of Minnesota. The jejunoileal bypass (JIB) induced a state of malabsorption by bypassing most of the intestines while keeping the stomach intact. Although the weight loss with the JIB was good, too many patients developed complications such as diarrhea, night blindness (from vitamin A deficiency), osteoporosis (from vitamin D deficiency), protein-calorie malnutrition, and kidney stones. Some of the most worrisome complications were associated with the toxic overgrowth of bacteria in the bypassed intestine. These bacteria then caused liver failure, severe arthritis, skin problems, and flu-like symptoms. Consequently, many patients have required reversal of the procedure.
The JIB is no longer a recommended bariatric surgical procedure. The lessons learned from the JIB include the crucial importance of long-term follow-up and the dangers of a permanent, severe and global malabsorption. Long-term follow-up by experienced bariatric surgeons is strongly recommended for all patients who have had a JIB in the past.
Chapter 3 – Gastric Bypass
Drs. Mason and Ito initially developed this procedure in the 1960s. The gastric bypass was based on the weight loss observed among patients undergoing partial stomach removal for ulcers. Over several decades, the gastric bypass has been modified into its current form, using a Roux-en-Y limb of intestine (RYGBP). The RYGBP is the most commonly performed operation for weight loss in the United States. In the U.S, approximately 140,000 gastric bypass procedures will be performed in 2005, far outnumbering the LAP-BAND®, duodenal switch, and vertical banded gastroplasty procedures.
Initially the operation was performed as a loop bypass with a much larger stomach. Because of bile reflux that occurred with the loop configuration, the operation is now performed as a “Roux-en-Y” with a limb of intestine connected to a very small stomach pouch which prevents the bile from entering the upper part of the stomach and esophagus.
The remaining stomach and first segment of small intestine are bypassed. In the standard RYGBP, the amount of intestine bypassed is not enough to create malabsorption of protein or other macronutrients. However, because the bypassed portion of intestine is where the majority of calcium and iron absorption takes place, anemia and osteoporosis are the most common long-term complications of the RYGBP. Therefore, lifelong mineral supplementation is mandatory. Other clinically important deficiencies that may occur include deficiencies of Vitamin B 1 (thiamine) and Vitamin B 12. Lifelong follow-up with a bariatric program and daily multi-vitamins are strongly recommended prevent nutritional complications.
The RYGBP has been proven in numerous studies to result in durable weight loss and an improvement in weight-related medical illnesses. Half of the weight loss often occurs during the first six months after surgery; weight loss usually peaks at 18-24 months. The obesity-related comorbidities that may be improved or cured with the RYGBP include diabetes mellitus of the adult onset type (so-called insulin resistant), hypertension, high cholesterol, arthritis, venous stasis disease, bladder incontinence, liver disease, certain types of headaches, heartburn, sleep apnea and many other disorders. Furthermore, the RYGBP has resulted in marked improvements in quality of life.
Although the most commonly performed RYGBP (sometimes called the proximal gastric bypass) involves little malabsorption, some surgeons modify the RYGBP to incorporate an element of malabsorption for the purpose of augmenting weight loss in special circumstances. This modification is sometimes called a distal gastric bypass, which may result in more severe nutritional complications than the proximal RYGBP . Whether long-term weight loss is superior to the proximal RYGBP or whether the malabsorptive complications are worth the possible improvements in weight loss has not been well established . Many surgeons reserve the distal RYGBP for very select circumstances.
The mechanism in which the RYGBP works is complex. After surgery, patients often experience marked changes in their behavior. Most patients have a reduction in hunger and feel full sooner after eating. Patients often state that they enjoy healthy foods and lose many of their improper food cravings. Rarely do people feel deprived of food. These complex behavioral changes are partially due to alterations in several hormones (ghrelin, GIP, GLP, PYY) and neural signals produced in the GI tract that communicate with the hunger centers in the brain. Another mechanism for weight loss after the RYGBP is referred to as the dumping syndrome. Dumping may result in lightheadedness, flushing, heart palpitations, diarrhea and other symptoms early (within 10 to 30 minutes) after eating sweets or foods with a high concentration of sugar. Some people remain extremely sensitive to sweets for the rest of their lives; most patients lose some or all of their sweets sensitivity over time.
The risk of dying in the first month after a RYGBP from complications of the operation is about 0.2 to 0.5% in expert centers. Studies have demonstrated that the mortality rate from hospitals with a low experience with the procedure is far higher than that reported by expert centers. The American Society of Bariatric Surgeons fully supports the initiative of the Surgical Review Committee to establish rigid criteria to certify that hospitals with quality programs will be designated as a “Center of Excellence.”
Advantages of RYGBP:
- Better weight loss than after purely restrictive procedures
- Low incidence of protein-calorie malnutrition and diarrhea
- Rapid improvement or resolution of weight-related comorbidities
- Appetite reduction
Complications of RYGBP:
COLUMNS
Early:
Anastomotic Leak
Pulmonary embolism
Wound infection
Gastrointestinal hemorrhage
Respiratory insufficiency
Mortality
Late:
Incisional hernia
Bowel obstruction
Internal hernia
Stomal stenosis
Micronutrient deficiencies
Marginal ulcer
Laparoscopic Gastric Bypass
Although the open RYGBP can be performed with a relatively low morbidity and mortality, the wound-related complications such as infection and incisional hernia can be troublesome. Wound infection occurs in as many as 8% of patients after open RYGBP and late incisional hernia occurs in as many as 20% of patients. However, some surgeons have reported a much lower rate. The laparoscopic approach to RYGBP was initiated in an effort to improve the early outcomes including a reduction in postoperative complications arising from a large incision in a severely obese patient.
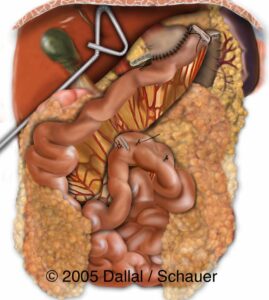
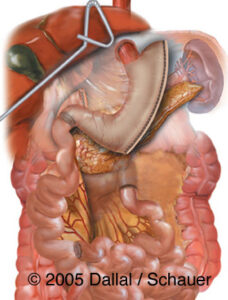
In 1994, Drs. Wittgrove and Clark reported the first case series of laparoscopic RYGBP. The primary differences between laparoscopic and open RYGBP are the method of access and method of exposure. Laparoscopic RYGBP is normally performed through 5-6 small abdominal incisions (0.5-2.0 cm), the peritoneal cavity (abdomen) is insufflated with carbon dioxide gas which creates a space within which to work, allowing exposure of the operative field. In contrast, open RYGBP is performed through a larger incision and abdominal wall retractors are used for exposure. By reducing the size of the surgical incision and the trauma associated with the operative exposure, the surgical insult has been shown to be less after laparoscopic compared to open RYGBP. However, not all patients are candidates for a laparoscopic approach based on body habitus, previous intra-abdominal surgery, etc.
Clinical studies have demonstrated that laparoscopic RYGBP is a safe and effective alternative to open RYGBP for the treatment of morbid obesity. Higa and colleagues reported the largest laparoscopic RYGBP experience with 1,500 operations. There have been three prospective, randomized trials comparing the outcomes of laparoscopic vs open RYGBP. The largest trial was reported by Nguyen and colleagues in 2001. In 2004, a group from Murcia, Spain published their results. Long-term weight loss after laparoscopic and open RYGBP should not differ, as the primary differences between the two techniques is largely in the method of access and not the gastrointestinal reconstruction.
Despite the advantages of the laparoscopic approach, open bariatric surgery still plays a prominent role in management of morbidly obese patients. Relative contraindications for laparoscopic bariatric surgery include patients with extremely high body mass index, patients with multiple previous upper abdominal surgeries, and patients with prior bariatric surgery. Another limitation of the laparoscopic approach is the steep learning curve of this technically challenging procedure for the surgeon, so it is not an operation for the surgeon who has not been trained specifically in this technique. The advantages and disadvantages of laparoscopic RYGBP are listed below.
Advantages of laparoscopic compared to open RYGBP
- Lesser intraoperative blood loss
- Shorter hospitalization
- Reduced postoperative pain
- Less pulmonary complications (atelectasis)
- Faster recovery
- Better cosmesis
- Fewer wound complications (incisional hernias and infections)
Disadvantages of laparoscopic compared to open RYGBP
- Complex laparoscopic operation associated with a steep learning curve
- Possible increase in the rate of internal hernia
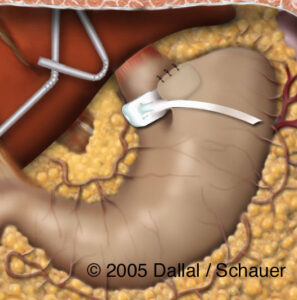
Silastic® ring gastric bypass
The Silastic® ring gastric bypass is a banded pouch RYGBP. A Silastic® ring is placed around the vertically constructed gastric pouch above the anastomosis between the pouch and intestinal Roux limb. The band controls stoma size by prevention of dilatation of the gastric pouch outlet, and is thought to provide better long-term control of the rate of emptying of the pouch and caloric intake. This procedure also includes placement of a gastrostomy tube for decompression of the distal stomach; a radio-opaque ring marker may be placed around the gastrostomy site to facilitate future percutaneous access to the distal stomach. A small percentage (3%) of patients may have band erosion or obstruction, necessitating reoperations and band removal.
Chapter 4. Biliopancreatic Diversion and Duodenal Switch
Biliopancreatic Diversion
Scopinaro first performed the biliopancreatic diversion (BPD) which was designed to be a safer malabsorptive alternative to the JIB. This operation induces controlled malabsorption without many of the potential side effects caused by bacterial overgrowth associated with the JIB. The m alabsorptive operations differ from the RYGBP and the gastric banding, which work mainly through restriction.
Malabsorption is defined by the incomplete uptake of calories and nutrients and occurs via two mechanisms. First, the bile and pancreatic fluids released into the duodenum to digest food and break down fats, carbohydrates and proteins are diverted away from ingested food – hence the name, biliopancreatic diversion. The digestive enzymes eventually join the ingested food – but at a point in the distal small intestine (ileum) where there is much less chance for complete breakdown and absorption. When food is in the diverted small intestine it is not absorbed as well because of the lack of enzymes to break down the larger fat, protein and carbohydrate molecules into their smaller building blocks, the actual particles absorbed. Because of the particular digestive aids necessary to absorb fats (bile and lipase are crucial), fat calorie malabsorption predominates. Unfortunately, undigested fats cause gas and loose, foul-smelling bowel movements, called steatorrhea. The second mechanism through which malabsorption occurs is by decreasing the amount of small intestine through which the ingested food passes. With less surface area of intestine with which food is in contact, less nutrients can be absorbed.
Unlike the RYGBP where no stomach is removed (only bypassed), the BPD involves the removal of 70% of the stomach. This procedure is done to decrease the amount of acid produced by the remaining stomach. Gastrin, a hormone produced by G-cells in the antrum, is responsible for stimulating the upper stomach to produce acid. Of note, the portion of the remaining upper stomach is far larger than the small “pouch” created for the RYGBP. This allows patients to eat larger volumes than after a restrictive operation before feeling full (satiety). After entering the upper stomach, food passes through a newly created connection (anastomosis) into the small intestine (alimentary limb). This anatomy is very similar in principle to the standard RYGBP, except that the length of the intestine from the stomach to the colon is much shorter – promoting malabsorption. The bile and pancreatic secretions pass through the bypassed biliopancreatic channel and connect with the alimentary channel (where the food travels) 50-100 cm from the colon. Some of these secretions are reabsorbed in this channel prior to meeting the alimentary tract. The part of the intestines where bile and pancreatic fluids (from the biliopancreatic channel) and food (from the alimentary channel) mix is called the common channel. Surgeons use various formulas to determine the appropriate length of the alimentary channel and the common channel.
The amount of excess weight loss after the BPD has been reported to be around 70 percent – with weight loss in some patients persisting up to 18 years. However, like all weight loss data, this percentage of excess weight lost varies depending on the length of follow-up, the quality of follow-up, the country where the procedure was performed, the surgeon, and the initial weight of the patient. Being a malabsorption operation, however, the BPD requires life-long medical follow-up.
Duodenal Switch
The duodenal switch (DS) is a modification of the BPD designed to prevent ulcers, increase the amount of gastric restriction, minimize the incidence of dumping syndrome, and reduce the severity of protein-calorie malnutrition. However, the dumping syndrome is also believed by many to be a benefit, rather than a detriment, in that it helps patients avoid eating sugary and high fat foods which would adversely affect weight loss. The DS was first reported by Dr. Doug Hess in 1986.
The DS works through an element of gastric restriction as well as malabsorption. The stomach is fashioned into a small tube, preserving the pylorus, transecting the duodenum and connecting the intestine to the duodenum above where digestive juices enter the intestine. Compared to the BPD, the DS leaves a much smaller stomach that creates a feeling of restriction much like that of a RYGBP. Anatomically, the main difference between the DS and the BPD is the shape of the stomach – the malabsorptive component is essentially identical to that of the BPD. Instead of cutting the stomach horizontally and removing the lower half (such as with the BPD), the DS cuts the stomach vertically and leaves a tube of stomach that empties into a very short (2-4 cm) segment of duodenum.
The duodenum is tolerant of stomach acid and therefore is much more resistant to ulceration compared to the small intestine. Removing part of the stomach also decreases the amount of acid present. Whereas the BPD involves an anastomosis (connection) between the stomach and the intestine, the DS involves an anastomosis between the duodenum and the intestine. The duodenum is cut about 2-4 cm from the stomach (measured from the pyloric valve). The intestine is sewn to the end of the duodenum which remains in continuity with the stomach. The other side of the duodenum will carry all the bile and pancreatic secretions. A theoretical (but clinically unproven) benefit of the DS is an improvement in absorption of iron and calcium in comparison to the BPD. The disadvantage of transecting the duodenum is the large number of vital structures immediately adjacent to the duodenum. Several large blood vessels and the major bile duct are located here. Injury to these structures can be life-threatening.
These procedures have some of the highest reported weight loss in long-term studies, but also have the highest rate of nutritional complications compared to the RYGBP and the purely restrictive procedures. These operations are some of the most complex in bariatric surgery. However, as with most studies of weight loss surgery, there is wide variability in long-term results between different centers. Only multi-center comparative studies can establish definitively the true differences between all these operations.
Some patients and surgeons believe that the DS is a superior operation to the RYGBP and BPD because of the lack of a “dumping syndrome”, described above. The DS and BPD have their own particular side effects. After a meal that is high in fat, people can experience foul smelling gas and diarrhea.
Advantages of BPD and DS:
- Increased amount of food intake compared to the bypass and band
- Less food intolerance
- Possibly greater long-term weight loss
- More rapid weight loss compared with gastric banding procedures
Complications of BPD and DS:
- Diarrhea and foul smelling gas, with an average of 3-4 loose bowel movements a day
- Malabsorption of fat soluble vitamins (Vitamins A, D, E, and K)
- Vitamin A deficiency, which causes night blindness
- Vitamin D deficiency, which causes osteoporosis
- Iron deficiency –a similar incidence with the RYGBP
- Protein-calorie malnutrition, which might require a second operation to lengthen the common channel
- Ulcers (less frequent with DS)
- Dumping syndrome (less frequent with DS)
Summary
Both the BPD and the DS can be performed laparoscopically. However, these operations are more demanding technically than the RYGBP and should only be performed in the most experienced hands. Long-term follow up and daily vitamin supplements are crucial to the success of these operations. Life-long monitoring is necessary to prevent nutritional and mineral deficiencies – just as with the RYGBP.
Chapter 5 – Gastroplasty
The gastroplasty was designed in the early 1970s to be a safer alternative to the RYGBP and the JIB. The operation itself was made possible by the introduction of mechanical staplers. The gastroplasty was the first purely restrictive operation performed for the treatment of obesity. The original (horizontal) gastroplasty involved stapling the stomach into a small partition – and only leaving a small opening for food to pass from the upper stomach pouch to the lower one. Thus the lay term – stomach stapling. This form of gastroplasty resulted in very poor long-term weight loss and, after several attempted modifications, was abandoned eventually.

The vertical banded gastroplasty (VBG) features a pouch based on the lesser curvature of the stomach and a polypropylene mesh band or Silastic® ring around the outlet of the pouch. The advantages of the VBG include a low mortality rate and the virtual absence of micronutrient deficiencies. Also, since no anastomosis is created, there is a lower risk of infectious complications.
However, once a very popular surgical option for obesity, the VBG is being performed much less frequently, because long-term studies have shown a prominent rate of weight regain or exacerbation of severe heartburn. Several randomized, prospective trials have demonstrated superior weight loss with RYGBP compared to VBG. Weight loss for sweets eaters has been shown to be superior with RYGBP compared to VBG, presumably as a result of symptoms of the dumping syndrome with sweets.
Chapter 6 – Gastric Banding and Laparoscopic Adjustable Gastric Banding
Gastric Banding
Another example of a purely restrictive bariatric procedure is nonadjustable gastric banding. It was first introduced in 1978 by Wilkinson, who applied a 2 cm Marlex mesh round the upper part of the stomach and separated the stomach into a small upper pouch and the rest of the stomach. Eventual pouch dilatation resulted in unsatisfactory weight loss.
In 1980, Molina described the gastric segmentation procedure, in which a Dacron vascular graft was placed around the upper stomach. The gastric pouch was smaller than Wilkinson’s procedure. Because the Dacron graft produced adherence of the liver to the band, it was replaced ultimately by PTFE (Gortex®).
In 1983, Kuzmak began using a 1 cm Silicone® band to encircle the stomach, creating a 13 mm stoma and a 30-50 mL proximal gastric pouch. This band was later modified to provide adjustability of the band diameter using an inflatable balloon (see below: “Laparoscopic adjustable gastric banding”).
Advantages of gastric banding
- Absence of anemia
- Absence of dumping
- Lack of malabsorption
- Short hospital stay
- Very low mortality rate
Complications of gastric banding
- Gastric perforation
- Incisional hernia
- Stomal stenosis
- Band slippage
- Band erosion into stomach
- Need for reversal or revision
Laparoscopic Adjustable Gastric Banding
he adjustable band was developed by Kuzmak who devised a Silicone® band lined with an inflatable balloon in 1986. This balloon was connected to a small reservoir that is placed under the skin of the abdomen through which the diameter of the band can be adjusted. Inflation of the balloon functionally tightens the band and thereby increases weight loss, while deflation of the balloon loosens the band and reduces weight loss. These bands can be inserted laparoscopically, thereby reducing the complications and discomfort of an open procedure.
Currently several brands of adjustable bands are available – the LAP-BAND ® System, the Swedish Adjustable Band and the Mid-Band. None have yet been shown clearly to be superior to the other. The LAP-BAND ® system (Inamed, Santa Barbara, CA) received US FDA approval in 2001.
Since these procedures do not involve an intestinal bypass, laparoscopic adjustable gastric banding (LAGB) is a procedure which induces weight loss solely through the restriction of food intake. For optimal results, strict patient compliance and frequent follow-up for band adjustments are required. The LAP-BAND ® is a reversible procedure that does not carry the risks of nutritional and mineral deficiencies of other bariatric procedures. The mortality risk with the LAGB is about 0.1% , which is less than that with the RYGBP.
The LAGB is safe and has a low rate of life-threatening complications. Excess weight loss with the laparoscopic adjustable gastric band is lower than that with the gastric bypass or malabsorptive procedures, varying between 28% and 65% at 2 years and 54% at 5 years. An improvement in weight-related comorbidities has been observed, including Type II diabetes mellitus, dyslipidemia, sleep apnea, gastroesophageal reflux, hypertension, and asthma. However, compared to the gastric bypass, the impact on co-morbidities appears to be somewhat less favorable. Remission of diabetes with LAGB is seen in 64-66% at one year and 80% at 2 yrs versus 93% at 9 years with RYGBP. Long-term results comparing LAGB with gastric bypass or BPD are not yet available.
While some studies have documented weight loss equal to RYGBP with fewer complications, other groups have had disappointing outcomes. Some studies document a substantial number of patients who have required re-operation for long-term complications of the adjustable band (such as for port problems, erosions and slippage, or inadequate weight loss). Conversion of a failed LAGB to another bariatric procedure may be technically more difficult and associated with more complications than with a first time RYGBP or DS operation.
Advantages of LAGB
- Same as gastric banding
- Adjustability of the band
- Reversibility (by band removal)
- Laparoscopic placement
Complications after LAGB
Intraoperative :
- Hemorrhage
- Injury to the spleen, stomach, or esophagus
- Conversion to open procedure
Postoperative :
- Band slippage (stomach prolapse)
- Leakage of the balloon or tubing
- Port Infection
- Band infection
- Obstruction
- Nausea and vomiting
Late complications
- Band erosion into the stomach
- Esophageal dilatation
- Failure to lose weight
References
Jejunoileal bypass
Kremen, AJ, Linner JH, et al. An experimental evaluation of the nutritional importance of proximal and distal small intestine. Ann Surg 1954;140:439-48.
Griffen Jr, WO, Bivins, BA, et al. The decline and fall of jejunoileal bypass. Surg Gynecol Obstet 1983;157:301-8.
Gastric Bypass
Mason, EE and Ito C. Gastric bypass in obesity. Surg Clin North Am 1967;47:1345-51.
MacDonald KG Jr, Long SD, Swanson MS,et al. The gastric bypass operation reduces the progression and mortality of non-insulin-dependent diabetes mellitus. J Gastrointest Surg 1997;1:213-220.
Sugerman HJ, Starkey JV, Birkenhauer R. A randomized prospective trial of gastric bypass versus vertical banded gastroplasty for morbid obesity and their effects on sweets versus non-sweets eaters. Ann Surg 1987;205:613-24.
Wittgrove AC, Clark GW, Tremblay LJ. Laparoscopic gastric bypass, Roux-en-Y: preliminary report of five cases. Obes Surg 4:353-357, 1994.
Higa KD, Ho T, Boone KB. Laparoscopic Roux-en-Y gastric bypass: technique and 3-year follow-up. J Laparoendosc Adv Surg Tech 2001;11:377-382.
Nguyen NT, Goldman C, Rosenquist CJ, et al: Laparoscopic versus open gastric bypass: a randomized study of outcomes, quality of life, and costs. Ann Surg 2001;234:279-289.
Lugan JA, Frutos D, Hernandez Q, et al. Laparoscopic versus open gastric bypass in the treatment of morbid obesity: a randomized prospective study. 2004;239:433-437.
Podnos YD, Jimenez JC, Wilson SE, Stevens M, Nguyen NT. Complications after laparoscopic gastric bypass. Arch Surg 2003;138:957-961.
Biliopancreatic diversion and duodenal switch
Scopinaro, N., Gianetta, E, et al. Biliopancreatic diversion for obesity at eighteen years. Surgery 1996;119:261-8.
Hess DS, Hess DW. Biliopancreatic diversion with a duodenal switch. Obes Surg 1998;8:267-82.
Marceau P, Hould FS, Simard S, et al. Biliopancreatic diversion with duodenal switch. World J Surg. 1998;22:947-54.
Gastroplasty
Mason, EE Vertical banded gastroplasty for obesity. Arch Surg 1982;117: 701-6.
Eckhout GV, Willbanks OL, Moore JT. Vertical ring gastroplasty for morbid obesity. Five year experience with 1,463 patients. Am J Surg 1986;152:713-6.
Gastric Banding
Oria, HE. Gastric banding for morbid obesity. Eur J Gastroenterol Hepatol 1999;11:105-114.
Kuzmak, LI, Yap, IS, McGuire L, et al. Surgery for morbid obesity. Using an inflatable gastric band. AORN J 1990;51:1307-24.
Belachew M, Belva PH, Desaive C. Long-term results of laparoscopic adjustable gastric banding for the treatment of morbid obesity. Obes Surg 2002;12:564-568.
O’Brien PE, Dixon JB, Brown W, et al. The laparoscopic adjustable gastric band (Lap-Band): a prospective study of medium-term effects on weight, health and quality of life. Obes Surg 2002;12:652-60.
Dixon JB, O’Brien PE. Health outcomes of severely obese type 2 diabetic subjects 1 year after laparoscopic adjustable gastric banding. Diabetes Care 2002;25:358-63.
Ponce J, Haynes B, Paynter S, et al. Effect of Lap-Band-induced weight loss on type 2 diabetes mellitus and hypertension. Obes Surg 2004;14:1335-42.