Prepared by Daniel Horwitz, B.S., M.S., John K. Saunders, M.D., Akuezunkpa Ude-Welcome, M.D., Manish Parikh, M.D.
Background: Many insurance companies require a medical weight management (MWM) program as a prerequisite for approval for bariatric surgery. There is debate regarding the benefit of this requirement. The objective of this study is to assess the effect of insurance-mandated MWM programs on weight loss outcomes in our bariatric surgery population.
Objective: To assess the effect of insurance-mandated MWM programs on weight loss outcomes in our bariatric surgery population.
Setting: University.
Methods: A retrospective review of all bariatric surgery cases performed between 2009 and 2013 was conducted. Patients were stratified by payor mix based on whether the insurance company required MWM. To control for differences between groups, a bucket matching algorithm was used to match patients based on gender, age, body mass index (BMI), and surgery type (sleeve gastrectomy, gastric bypass, or gastric band). A repeated-measures regression model was created to estimate percent excess weight loss, percent excess BMI loss, and percent total weight loss.
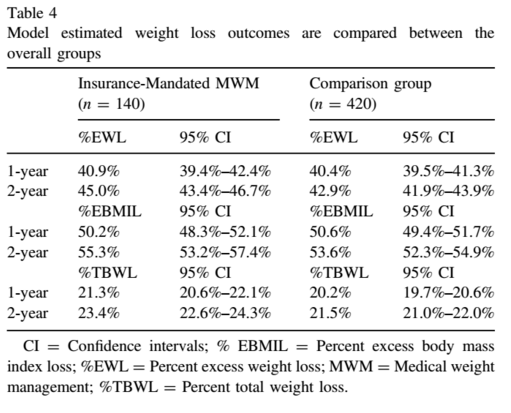
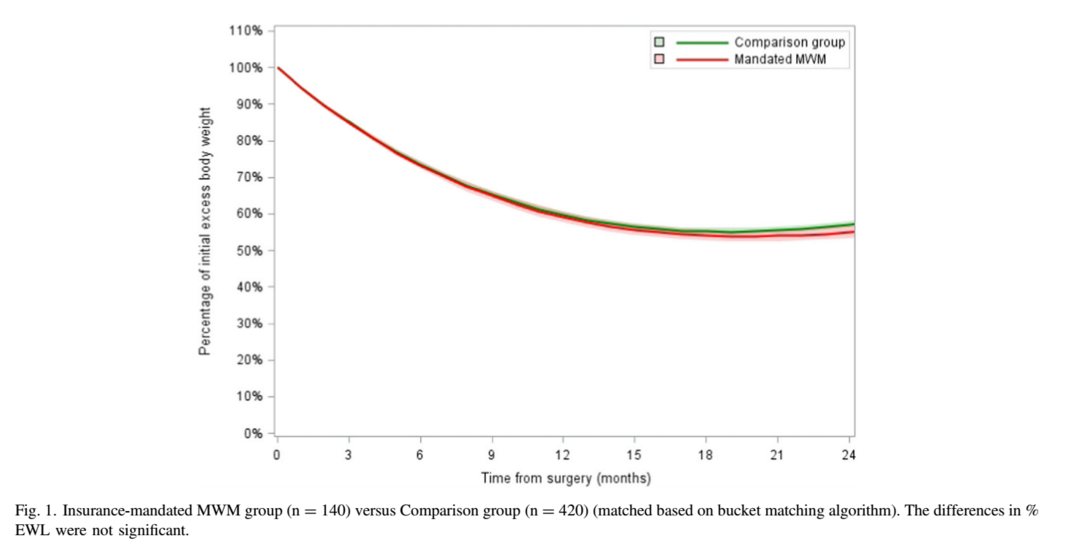
Results: A total of 1432 bariatric surgery patients were reviewed. The bucket-matching algorithm resulted in 560 patients for final analysis. Mean age and BMI were 41 years and 43 kg/m2 respectively, and 91% were female. The regression model found no significant differences in weight loss outcomes between the MWM group and the comparison group at 1 year and 2 years—percent total weight loss: 21.3% [95% confidence interval [CI] 20.6%–22.1%] versus 20.2% [95%CI 19.7%– 20.6%) at 1 year and 23.4% [95%CI 22.6%–24.3%] versus 21.5% [95%CI 21.0%–22.0%] at 2 years.
Conclusion: There was no difference in weight loss outcomes up to 2 years in patients who required insurance-mandated MWM programs. Longer-term studies are needed to determine the benefit of this insurance requirement. (Surg Obes Relat Dis 2016;12:496–501.) © 2016 American Society for Metabolic and Bariatric Surgery. All rights reserved.
Many insurance companies require that patients complete a medically-supervised weight management (MWM) program as a condition for approval for bariatric surgery [1]. Many bariatric surgery programs have undoubtedly enrolled patients whose surgery was eventually denied by insurance companies because of inadequate completion of MWM programs. Insurance-mandated MWM programs typically range from 4 to 6 months and require consecutive monthly documentation of weight and dietary counseling. Although mandatory preoperative weight loss, especially in the super-obese patients, may lead to better postoperative outcomes, it is unclear whether insurance-mandated MWM programs actually lead to weight loss [2]. Other studies have suggested that insurance-mandated MWM programs may increase the “drop-out” rate before bariatric surgery [3]. The purpose of this study is to retrospectively review patients undergoing bariatric surgery at our institution to compare outcomes between patients whose insurance required MWM with those whose insurance did not.
Materials and Methods
A retrospective review of all patients undergoing bariatric surgery at our institution between 2009 and 2013 was conducted. Institutional Review Board approval was obtained. All patients met the 1991 NIH consensus criteria for bariatric surgery [4]. Patients were stratified by payor mix on the basis of whether the insurance company required any MWM. All patients (regardless of insurance) completed program-specific requirements, including multidisciplinary evaluation by a psychologist, nutritionist, and surgeon and a preoperative liquid protein diet for at least 2 weeks.
Because there were inherent differences between the 2 groups, a bucket matching algorithm was applied to match 1 MWM patient to 3 controls to create the final cohort. Patients were matched based on gender, age, body mass index (BMI), and surgical procedure. A repeated-measures model was then generated to compare the estimated differences in percent excess weight loss (%EWL), percent excess body mass index loss, and percent total weight loss at 12 and 24 months. For men, ideal body weight (IBW) was calculated as IBW = 51.65kg þ 1.85 kg/inch of height greater than 5 feet. For women, IBW = 48.67 kg þ 1.65 kg/ inch of height greater than 5 feet [5]. An ideal BMI of 25 was assumed for all patients. χ2 and Fisher exact tests were used to compare groups, as appropriate.
Results
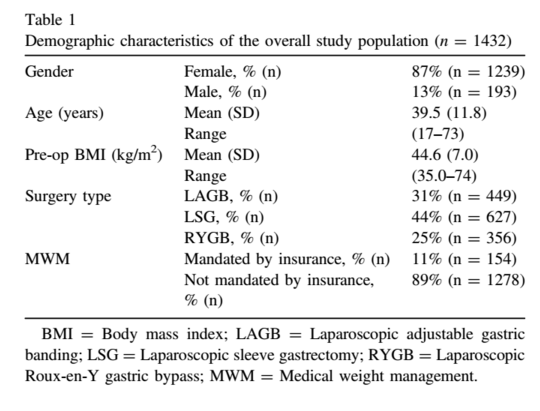
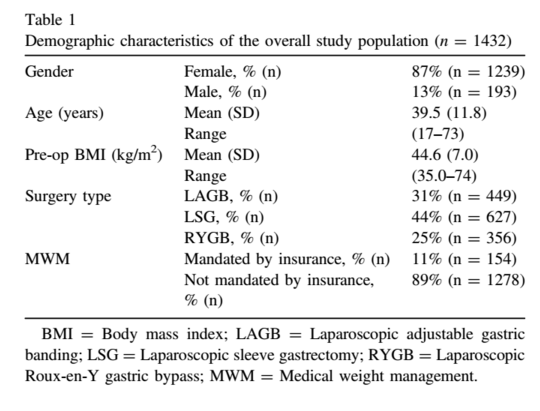
A total of 1432 bariatric surgery patients were reviewed for analysis. Demographic characteristics are shown in Table 1. Most patients (89%) were covered by insurance that did not require MWM. When stratifying by payor mix, the patients that had insurance that required MWM were slightly older (42 years versus 39 years, p = .0083) and represented a different mix of surgery types (Table 2).
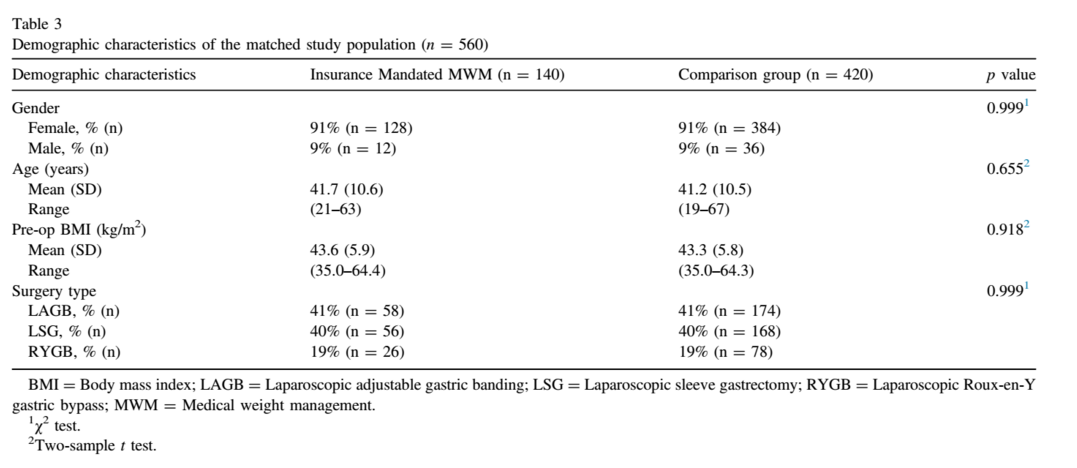
The bucket-matching algorithm resulted in a total sample size of 560 patients (140 MWM patients and 420 controls), consisting of gastric bands (41%), sleeve gastrectomies (40%), and gastric bypasses (19%). The demographic characteristics of the matched cohort are listed in Table 3. The matched groups were used to evaluate differences in % EWL, percent excess body mass index loss, and percent total weight loss at 1 and 2 years postsurgery. The repeated-measures model found no difference in weight loss out-
comes between the 2 groups at 1 and 2 years (Table 4 and Fig. 1).
Discussion
Many insurance companies require a set period of MWM (typically 4–6 months) as prerequisite for approval for bariatric surgery. The justification is presumably to enhance postoperative weight loss outcomes and ensure dietary compliance. This retrospective review utilized a bucket-matching algorithm to compare a cohort of 540 patients and found no major benefit of MWM programs on weight loss up to 2 years postoperatively.
This study adds to the existing literature regarding the overall lack of benefit for insurance-mandated MWM. In 2006, Jamal et al. retrospectively compared 72 gastric bypass patients who underwent mandatory MWM (13 weeks) to 252 patients who did not [3]. At 1 year follow-up, the non-MWM patients had higher %EWL (67% versus 60%, p <.0001). The MWM group had a higher dropout rate (28% versus 19%, p <.05). They concluded that insurance-mandated MWM programs have no benefit and may be an obstacle to patient access for bariatric surgery. In 2010, Ochner, Puma, Raevuori, Teixeira, and Geliebter compared 94 gastric bypass patients who underwent mandatory MWM (6 months) with 59 patients who did not [2]. They found that the 6-month MWM requirement was ineffective in reducing weight before surgery. Finally, we performed a small randomized study in 2008 of 55 patients who were randomized to 6 months of MWM versus usual care [6]. This study also found no change in postsurgical weight loss outcomes.
There is some data suggesting preoperative weight loss leads to improved clinical outcomes and less postoperative complications, particularly in the super-obese. A randomized trial evaluating the effect of a 10% weight loss requirement preoperatively found a decreased operative time and decreased 3-month %EWL but no change in 6 month %EWL [7]. Systematic reviews and meta-analyses regarding preoperative weight loss have shown that pre-operative weight loss may be associated with greater weight loss postoperatively [8,9]. Many centers, including ours, aim for some degree of preoperative weight loss, especially in the super-obese (BMI > 50 kg/m2 Usually, a 2-week liquid protein diet is adequate to achieve this. This is also perhaps more cost-effective than the resources required to sustain MWM programs (MWM clinicians, ancillary support, clinic space, patient travel time, and travel costs).
There were several limitations to this study. This was a retrospective study that consisted of significantly more patients whose insurance did not require MWM. Although the bucket-matching algorithm (1:3) was used to control for this mismatch, as well as the inherent differences between the 2 cohorts, there may have been other confounding factors for which we did not account. Nevertheless, this is one of the largest studies (n = 540) in this area and the only one that utilized a matching algorithm to attempt to control for inherent differences between the group. We also did not take into account the dropout rate of patients who enrolled in the MWM program but did not complete it (and thus did not undergo surgery). We also did not compare the varying lengths of the MWM programs (e.g., 4 months versus 6 months).
Conclusion
There was no difference in weight loss outcomes up to 2 years in patients who required insurance-mandated MWM programs. Longer-term studies are needed to determine the benefit of this insurance requirement.
Financial Disclosures
The authors have no financial disclosures.
References
[1] UnitedHealthcare [homepage on the Internet]. Minnetonka, Minnesota: UnitedHealth Group; c2011-2015 [cited 2015 June 1]. Bariatric Surgery Medical Policy; [about 34 screens]. Available www.unitedhealthcareonline.com/ccmcontent/ProviderII/UHC/en-US/Assets/ProviderStaticFiles/ProviderStaticFilesPdf/Tools%20and%20Resources/Policies%20and%20Protocols/Medical%20Policies/Medical%20Policies/Bariatric_Surgery.pdf.
[2] Ochner CN, Puma LM, Raevuori A, Teixeira J, Geliebter A. Effectiveness of a prebariatric surgery insurance-required weight loss regimen and relation to postsurgical weight loss. Obesity (Silver Spring) 2010;18(2):287–92.
[3] Jamal MK, DeMaria EJ, Johnson JM, et al. Insurance-mandated preoperative dietary counseling does not improve outcome and increases dropout rates in patients considering gastric bypass surgery for morbid obesity. Surg Obes Relat Dis 2006;2(2):122–7.
[4] National Institutes of Health. Gastrointestinal Surgery for Severe Obesity. Consens Statement 1991;9(1):1–20.
[5] Robinson J, Lupkiewicz S, Palenik L, Lopez LM, Ariet M. Determination of ideal body weight for drug dosage calculations. Am J Hosp Pharm 1983;40(6):1016–9.
[6] Parikh M, Dasari M, McMacken M, Ren C, Fielding G, Ogedegbe G. Does a preoperative medically supervised weight loss program improve bariatric surgery outcomes? A pilot randomized study. Surg Endosc 2012;26(3):853–61.
[7] Alami RS, Morton JM, Schuster R, et al. Is there a benefit to preoperative weight loss in gastric bypass patients? A prospective randomized trial. Surg Obes Relat Dis 2007;3(2):141–5. discussion 145–6.
[8] Livhits M, Mercado C, Yermilov I, et al. Does weight loss immediately before bariatric surgery improve outcomes: a systematic review. Surg Obes Relat Dis 2009;5(6):713–21.
[9] Livhits M, Mercado C, Yermilov I, et al. Preoperative predictors of weight loss following bariatric surgery: systematic review. Obes Surg 2012;22(1):70–89.