CONTACT: ASMBS@compartnersny.com
WASHINGTON, DC – June 17, 2025 – The higher a person’s body mass index (BMI), the higher their risk for complications after bariatric surgery, especially those with BMI of 50 or more, according to a new study presented today at the American Society for Metabolic and Bariatric Surgery (ASMBS) 2025 Annual Scientific Meeting.
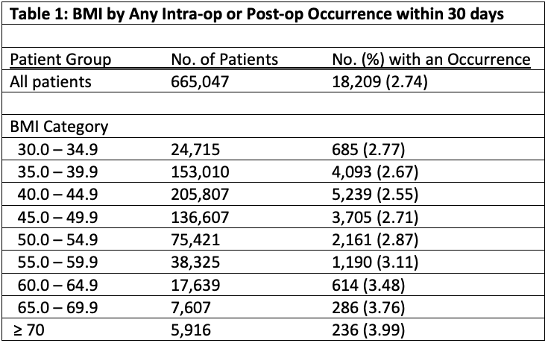
Researchers found that the rate of complications increased by an average of 5.56% and serious occurrences rose 3.21% from the lowest BMI category to the highest, with people with a BMI 50 or more the most likely to experience complications of any kind.
“The study gives new insights into the risks associated with each BMI category and identifies the inflection point for increased risk of morbidity and mortality, which occurs when patients pass BMI 50,” said study co-author John Scott, MD, FACS, FASMBS, Chief for the Division of Minimal Access and Bariatric Surgery for the Prisma Health Dept. of Surgery in Greenville, SC. “Obesity itself is a risk factor in surgeries of all kinds, but in bariatric surgery the risks remain relatively low.”
The retrospective study involved a review of the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP) database for patients with obesity (BMI 30 or more) who had either sleeve gastrectomy or Roux-en-Y gastric bypass between 2020 and 2023. A total of 665,047 cases were included.
“While complication rates are generally low, this study provides granular data not previously reported that can help withpre-operative counseling and to make surgery even safer and patient outcomes even better,” said Richard M. Peterson, MD, MPH, FACS, FASMBS, President-elect, ASMBS, and Professor of Surgery, UT Health San Antonio, who was not involved in the study.
About Metabolic and Bariatric Surgery
Metabolic, bariatric, or weight-loss surgery such as gastric bypass and sleeve gastrectomy has been shown to be the most effective and long-lasting treatment for severe obesity. The operations improve or resolve diseases including type 2 diabetes, heart disease and high blood pressure and leads to significant and durable weight loss. Its safety profile is comparable to some of the safest and most commonly performed surgeries in the U.S. including gallbladder surgery, appendectomy and knee replacement. The ASMBS reports more than 270,000 metabolic and bariatric procedures were performed in 2023, which represents only about 1% of those who meet eligibility requirements based on BMI.
About Obesity
According to the U.S. Centers for Disease Control and Prevention (CDC), the prevalence of obesity and severe obesity is 40.3% and 9.4%, respectively. Studies show the disease can weaken or impair the body’s immune system and cause chronic inflammation and increase the risk of scores of other diseases and conditions including cardiovascular disease, stroke, type 2 diabetes, and certain cancers.
About ASMBS
The ASMBS is the largest organization for bariatric surgeons in the United States. It is a non-profit organization that works to advance the art and science of bariatric surgery and is committed to educating medical professionals and the lay public about bariatric surgery as an option for the treatment of severe obesity, as well as the associated risks and benefits. It encourages its members to investigate and discover new advances in bariatric surgery, while maintaining a steady exchange of experiences and ideas that may lead to improved surgical outcomes for patients with severe obesity. For more information, visit www.asmbs.org.
###
*BARIATRIC SURGERY COMPLICATIONS BY BMI, A CONTINUED REVIEW AND ANALYSIS OF 2020-2023 NATIONAL MBSAQIP DATABASE Nicholas Dahlgren Prisma Health Academics; John Scott Prisma Health; Eugene Langan Geisinger Health; Peter Buccini Prisma Health Academics; Dawn Blackhurst Msingi Institute