Updated May 2021 | Written by the Public Education Committee
Weight loss surgery is also known as bariatric and metabolic surgery. These terms are used in order to reflect the impact of these operations on patients’ weight and the health of their metabolism (breakdown of food into energy). In addition to their ability to treat obesity, these operations are very effective in treating diabetes, high blood pressure, sleep apnea and high cholesterol, among many other diseases. These operations also have an ability to prevent future health problems. The benefits allow patients with obesity who choose to undergo treatment to enjoy a better quality of life and a longer lifespan.
Today’s metabolic and bariatric operations have been refined over the course of many decades and are among the best studied treatments in modern medicine. They are performed with small incisions using minimally invasive surgical techniques (laparoscopic and robotic surgery). These advancements allow patients to have a better overall experience with less pain, fewer complications, shorter hospital stays and a faster recovery. These operations are extremely safe, with complication rates that are lower than common operations such as gallbladder removal, hysterectomy, and hip replacement.
The goal of these operations is to modify the stomach and intestines to treat obesity and related diseases. The operations may make the stomach smaller and also bypass a portion of the intestine. This results in less food intake and changes how the body absorbs food for energy resulting in decreased hunger and increased fullness. These procedures improve the body’s ability to achieve a healthy weight.
The common procedures endorsed by the American Society for Metabolic and Bariatric Surgery are listed and explained below. Each surgery has its own advantages and potential drawbacks. Your bariatric surgeon will review your health history and work with you to determine which surgery is best for you.
Sleeve Gastrectomy
The Laparoscopic Sleeve Gastrectomy, often called the “sleeve”, is performed by removing approximately 80% of the stomach. The remaining stomach is the size and shape of a banana.
The Procedure
- The stomach is freed from organs around it.
- Surgical staplers are used to remove 80% of the stomach, making it much smaller.
How it Works
The new stomach holds less food and liquid helping reduce the amount of food (and calories) that are consumed. By removing the portion of the stomach that produces most of the “hunger hormone”, the surgery has an effect on the metabolism. It decreases hunger, increases fullness, and allows the body to reach and maintain a healthy weight as well as blood sugar control. The simple nature of the operation makes it very safe without the potential complications from surgery on the small intestine.
Advantages
- Technically simple and shorter surgery time
- Can be performed in certain patients with high risk medical conditions
- May be performed as the first step for patients with severe obesity
- May be used as a bridge to gastric bypass or SADI-S procedures
- Effective weight loss and improvement of obesity related conditions
Disadvantages
- Non-reversible procedure
- May worsen or cause new onset reflux and heart burn
- Less impact on metabolism compared to bypass procedures
Roux-en-Y Gastric Bypass (RYGB)

The Roux-en-Y Gastric Bypass, often called the “gastric bypass”, has now been performed for more than 50 years and the laparoscopic approach has been refined since 1993. It is one of the most common operations and is very effective in treating obesity and obesity related diseases. The name is a French term meaning “in the form of a Y”.
The Procedure
- First, the stomach is divided into a smaller top portion (pouch) which is about the size of an egg. The larger part of the stomach is bypassed and no longer stores or digests food.
- The small intestine is also divided and connected to the new stomach pouch to allow food to pass. The small bowel segment which empties the bypassed or larger stomach is connected into the small bowel approximately 3-4 feet downstream, resulting in a bowel connection resembling the shape of the letter Y.
- Eventually the stomach acids and digestive enzymes from the bypassed stomach and first portion of the small intestine will mix with food that is eaten.
How it Works
The gastric bypass works in several ways. Like many bariatric procedures, the newly created stomach pouch is smaller and able to hold less food, which means fewer calories are ingested. Additionally, the food does not come into contact with the first portion of the small bowel and this results in decreased absorption. Most importantly, the modification of the food course through the gastrointestinal tract has a profound effect to decrease hunger, increase fullness, and allow the body to reach and maintain a healthy weight. The impact on hormones and metabolic health often results in improvement of adult onset diabetes even before any weight loss occurs. The operation also helps patients with reflux (heart burn) and often the symptoms quickly improve. Along with making appropriate food choices, patients must avoid tobacco products and non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen and naproxen.
Advantages
- Reliable and long-lasting weight loss
- Effective for remission of obesity-associated conditions
- Refined and standardized technique
Disadvantages
- Technically more complex when compared to sleeve gastrectomy or gastric band
- More vitamin and mineral deficiencies than sleeve gastrectomy or gastric banding
- There is a risk for small bowel complications and obstruction
- There is a risk of developing ulcers, especially with NSAID or tobacco use
- May cause “dumping syndrome”, a feeling of sickness after eating or drinking, especially sweets
Adjustable Gastric Band (AGB)
The Adjustable Gastric Band is a device made of silicone that is placed around the top part of the stomach to limit the amount of food a person can eat. It has been available in the United States since 2001. The impact on obesity related diseases and long-term weight loss is less than with other procedures. Its use has therefore declined over the past decade.
The Procedure

- This device is placed and secured around the top part of the stomach creating a small pouch above the band.
How it Works
The feeling of fullness depends upon the size of the opening between the pouch and the rest of the stomach. The opening size can be adjusted with fluid injections through a port underneath the skin. Food goes through the stomach normally but is limited by the smaller opening of the band. It is less successful against type 2 diabetes and has modest effects on the metabolism.
Advantages
- Lowest rate of complications early after surgery
- No division of the stomach or intestines
- Patients can go home on the day of surgery
- The band can be removed if needed
- Has the lowest risk for vitamin and mineral deficiencies
Disadvantages
- The band may need several adjustments and monthly office visits during the first year
- Slower and less weight loss than with other surgical procedures
- There is a risk of band movement (slippage) or damage to the stomach over time (erosion)
- Requires a foreign implant to remain in the body
- Has a high rate of re-operation
- Can result in swallowing problems and enlargement of the esophagus
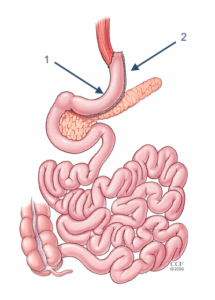
Biliopancreatic Diversion with Duodenal Switch (BPD/DS)

The Biliopancreatic Diversion with Duodenal Switch, abbreviated BPD-DS, begins with creation of a tube-shaped stomach pouch similar to the sleeve gastrectomy. It resembles the gastric bypass, where more of the small intestine is not used.
The Procedure
- Following creation of the sleeve-like stomach, the first portion of the small intestine is separated from the stomach.
- A part of the small intestine is then brought up and connected to the outlet of the newly created stomach, so that when the patient eats, the food goes through the sleeve pouch and into the latter part of the small intestine.
How it Works
The smaller stomach, shaped like a banana, allows patients to eat less food. The food stream bypasses roughly 75% of the small intestine, the most of any commonly performed approved procedures. This results in a significant decrease in the absorption of calories and nutrients. Patients must take vitamins and mineral supplements after surgery. Even more than gastric bypass and sleeve gastrectomy, the BPD-DS affects intestinal hormones in a manner that reduces hunger, increases fullness and improves blood sugar control. The BPD-DS is considered to be the most effective approved metabolic operation for the treatment of type 2 diabetes.
Advantages
- Among the best results for improving obesity
- Affects bowel hormones to cause less hunger and more fullness after eating
- It is the most effective procedure for treatment of type 2 diabetes
Disadvantages
- Has slightly higher complication rates than other procedures
- Highest malabsorption and greater possibility of vitamins and micro-nutrient deficiencies
- Reflux and heart burn can develop or get worse
- Risk of looser and more frequent bowel movements
- More complex surgery requiring more operative time
Single Anastomosis Duodeno-Ileal Bypass with Sleeve Gastrectomy (SADI-S)
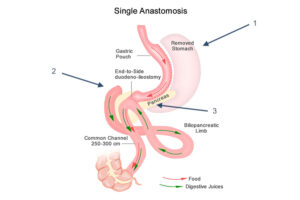
The Single Anastomosis Duodenal-Ileal Bypass with Sleeve Gastrectomy, referred to as the SADI-S is the most recent procedure to be endorsed by the American Society for Metabolic and Bariatric Surgery. While similar to the BPD-DS, the SADI-S is simpler and takes less time to perform as there is only one surgical bowel connection.
The Procedure
- The operation starts the same way as the sleeve gastrectomy, making a smaller tube-shaped stomach.
- The first part of the small intestine is divided just after the stomach.
- A loop of intestine is measured several feet from its end and is then connected to the stomach. This is the only intestinal connection performed in this procedure.
How it Works
When the patient eats, food goes through the pouch and directly into the latter portion of the small intestine. The food then mixes with digestive juices from the first part of the small intestine. This allows enough absorption of vitamins and minerals to maintain healthy levels of nutrition. This surgery offers good weight loss along with less hunger, more fullness, blood sugar control and diabetes improvement.
Advantages
- Highly effective for long-term weight loss and remission of type 2 diabetes
- Simpler and faster to perform (one intestinal connection) than gastric bypass or BPD-DS
- Excellent option for a patient who already had a sleeve gastrectomy and is seeking further weight loss
Disadvantages
- Vitamins and minerals are not absorbed as well as in the sleeve gastrectomy or gastric band
- Newer operation with only short-term outcome data
- Potential to worsen or develop new-onset reflux
- Risk of looser and more frequent bowel movements
Summary
All of the procedures discussed above are endorsed by the American Society for Metabolic and Bariatric Surgery and are excellent options to help you achieve healthy, long-term weight loss and improve medical conditions related to obesity. While all operations have risks, bariatric procedures performed at accredited centers are safe and have a low risk for complications. Successful bariatric surgery requires a team-based approach including your surgeon, dietitian, psychologist, nurse case manager, and obesity medicine specialist who will focus on taking you through each step of the journey. Patients will do better if they continue to eat healthy, engage in physical activity, keep their appointments with obesity medicine providers, and take vitamins and mineral supplements as instructed. Your bariatric care team will provide you with lifelong support to succeed and maintain a permanent healthy lifestyle including changes to your diet and regular physical activity. Most patients need periodic blood work testing to monitor vitamin and mineral levels and have yearly checkups at their comprehensive metabolic and bariatric surgery care center.
Click here to find an ASMBS surgeon or healthcare provider near you: Find a Provider